Cystoceles is a prevalent condition among women, especially those who’ve experienced vaginal childbirth, multiple pregnancies, or entered postmenopause. Resolving the complexities of Cystocele, or prolapsed bladder, where weakened supportive tissues lead to discomfort, pelvic pressure, and urinary incontinence is a big deal. In this article, we are going to explore different types of Cystocele, their symptoms, causes, and diagnostic methods. Learn about personalized treatment options, from pelvic floor exercises to surgery, tailored to individual needs. Understanding and addressing Cystoceles starts here.
What is Cystoceles?
Cystocele, also known as a prolapsed bladder, is a condition in which the supportive tissues between a woman’s bladder and vagina weaken, causing the bladder to sag or droop into the vagina. This can result in discomfort, a feeling of pressure or fullness in the pelvic area, difficulty emptying the bladder, and urinary incontinence.
Different types of Cystoceles
There are several different types of cystocele, which are classified based on the location and severity of the prolapse. These include:
- Anterior cystocele: This is the most common type of cystocele, in which the bladder bulges into the front wall of the vagina.
- Posterior cystocele: In this type of cystocele, the rectum bulges into the back wall of the vagina.
- Apical cystocele: This type of cystocele occurs when the uterus or top of the vagina bulges down into the vaginal canal.
- Paravaginal cystocele: In this type of cystocele, the bladder bulges to one side of the vaginal wall.
The type of cystocele a woman has will determine the most appropriate treatment plan, as well as the likelihood of experiencing symptoms such as urinary incontinence or difficulty emptying the bladder. Treatment options may include pelvic floor exercises, pessary placement, estrogen therapy, or surgery, depending on the severity of the condition and the woman’s situation.
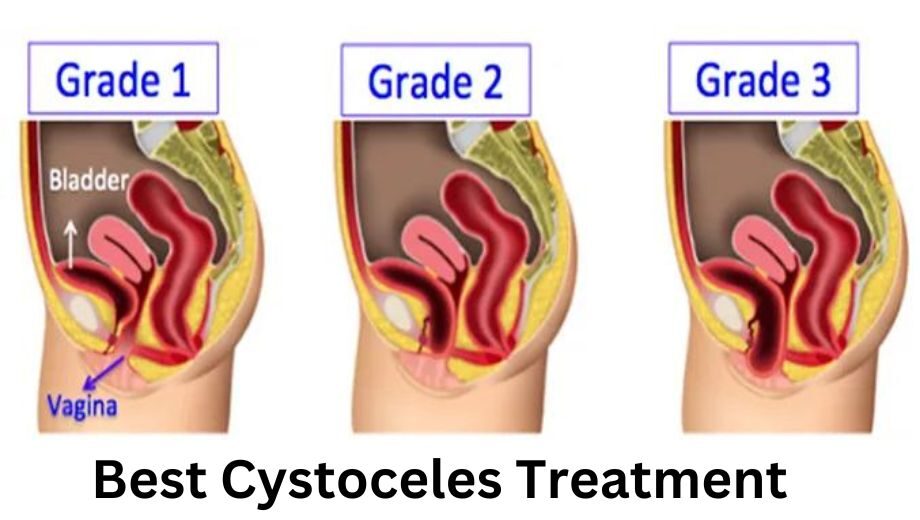
Different Grades of Cystoceles
Cystoceles, also known as prolapsed bladders, are often classified into grades to indicate the severity of the condition. The grading system typically ranges from Grade I to Grade IV, with each grade reflecting the extent of the prolapse. Here are the cystocele grades as follows
- Grade I: Mild prolapse, where the bladder descends slightly into the vagina but remains near its normal position.
- Grade II: Moderate prolapse, characterized by a more noticeable descent of the bladder into the vagina.
- Grade III: Severe prolapse, indicating a significant descent of the bladder to the opening of the vagina.
- Grade IV: Complete prolapse, where the bladder protrudes through the vaginal opening.
These grades help healthcare professionals assess the severity of the condition and tailor treatment plans accordingly. It allows for a more precise understanding of the impact on a patient’s quality of life and aids in determining the most appropriate interventions, ranging from lifestyle modifications and pelvic exercises to surgical options, depending on the grade of the cystocele.
Signs and Symptoms of Cystoceles
The signs and symptoms of cystoceles can vary depending on the severity of the condition but may include:
- A feeling of pressure or fullness in the pelvic area
- Bulging or protrusion of tissue into the vagina
- Urinary incontinence, including leaking urine when laughing, coughing, or sneezing
- Difficulty emptying the bladder completely
- Recurrent urinary tract infections
- Pain during sexual intercourse
- Back pain
- Constipation or difficulty passing stool
- A noticeable bulge or lump in the vaginal area
- A feeling of discomfort or pulling in the pelvic area
It is important for women who experience any of these symptoms to seek medical attention. A healthcare provider can perform a physical examination and may recommend additional testing or imaging to diagnose the condition and determine the most appropriate treatment plan.
Causes of Cystoceles
Cystoceles occur when the supportive tissue between a woman’s bladder and vagina weakens, causing the bladder to sag or droop into the vagina. The exact cause of this weakening is not always clear, but several factors may contribute to the development of cystoceles, including:
- Pregnancy and childbirth: The pelvic floor muscles and tissues can become stretched and weakened during pregnancy and childbirth, particularly during vaginal delivery.
- Aging: As women age, their pelvic floor muscles and tissues can naturally weaken, which can increase the risk of developing a cystocele.
- Menopause: The loss of estrogen that occurs during menopause can lead to changes in the pelvic floor muscles and tissues, which can increase the risk of developing a cystocele.
- Obesity: Excess weight can put increased pressure on the pelvic floor muscles and tissues, which can contribute to the development of a cystocele.
- Chronic constipation: Straining during bowel movements can put pressure on the pelvic floor muscles and tissues, which can weaken them over time.
- Chronic coughing: Frequent coughing can put pressure on the pelvic floor muscles and tissues, which can contribute to the development of a cystocele.
- Heavy lifting: Repeatedly lifting heavy objects can strain the pelvic floor muscles and tissues, which can increase the risk of developing a cystocele.
Method to diagnose Cystoceles
The diagnosis of cystoceles typically begins with a physical examination by a healthcare provider, which may include a pelvic exam. During the exam, the healthcare provider may ask the patient to bear down or cough, which can help to reveal any prolapse of the bladder or other pelvic organs. In addition to the physical exam, other tests may be used to diagnose cystoceles, including:
- Urinalysis: A urine sample may be collected to check for signs of infection or other abnormalities.
- Cystourethroscopy: This is a procedure that involves using a thin, flexible tube with a camera and light on the end to examine the inside of the bladder and urethra.
- Cystography: This is a type of X-ray that uses contrast dye to visualize the bladder and urethra.
- Magnetic resonance imaging (MRI): This is a type of imaging that uses a magnetic field and radio waves to create detailed images of the bladder and other pelvic organs.
- Electromyography (EMG): This is a test that measures the electrical activity of the muscles and nerves in the pelvic floor.
Treatment option for Cystoceles
The treatment for cystoceles will depend on the severity of the condition and the individual patient’s symptoms and medical history. Treatment options may include:
- Pelvic floor exercises: These exercises, also known as Kegels, can help to strengthen the pelvic floor muscles and improve bladder control. A physical therapist or other healthcare providers can guide how to perform these exercises correctly.
- Pessary placement: A pessary is a device that is inserted into the vagina to support the bladder and other pelvic organs. Pessaries come in a variety of shapes and sizes and can be fitted by a healthcare provider.
- Estrogen therapy: Estrogen therapy also known as cystocele therapies, either in the form of topical cream or oral medication, may be used to improve the strength and flexibility of the pelvic floor muscles and tissues.
- Surgery: In more severe cases of cystoceles, surgery may be necessary to repair the pelvic floor muscles and support the bladder and other pelvic organs. The specific surgical procedure used will depend on the individual patient’s needs and medical history.
Conclusion
Women need to discuss their treatment options with a healthcare provider to determine the most appropriate course of action. In many cases, a combination of different treatments may be used to achieve the best results. You can contact Dr. Ranjana who is one of the best gynecologists in Mumbai.